Endometriosis
Definition
A disease in which endometrial glands and stroma implant and are active in areas outside the uterus (ectopic endometrium)
Most commonly implants are found in the pelvis
Lesions may occur at far off sites like pleural cavity, liver, kidney, gluteal muscles, bladder etc.
Incidence
Familial
More common in women with infertility
5% of women in the reproductive age group
25% in infertile women
50% in chronic pelvic pain
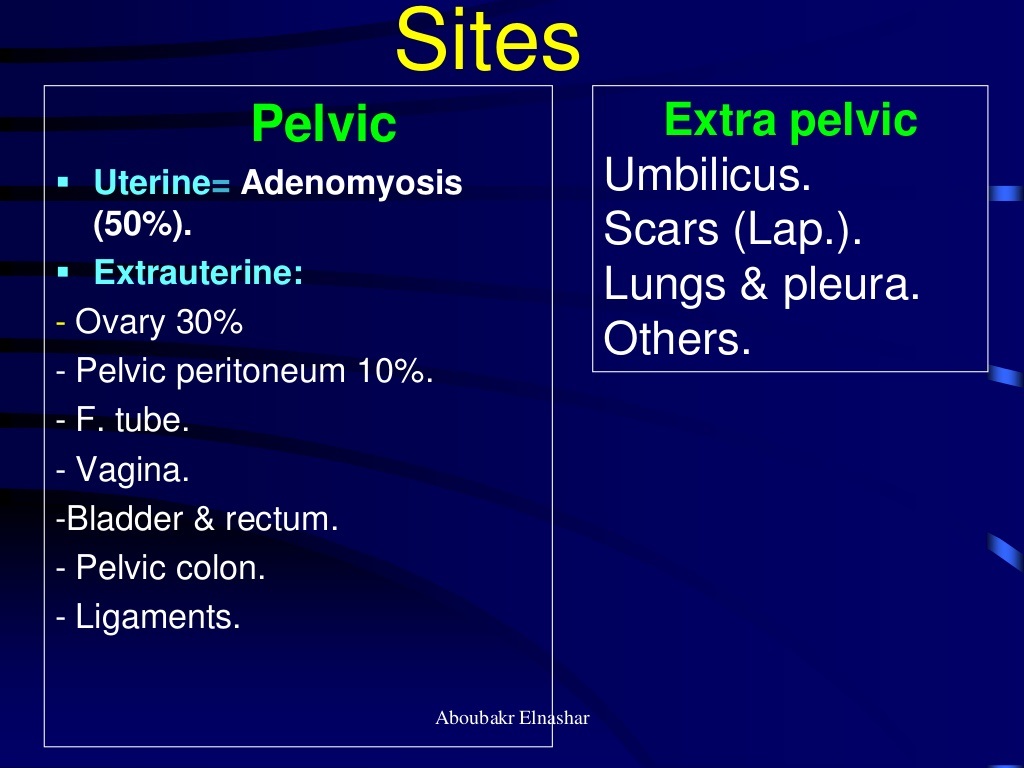
50% of endometriosis occurs in the myomatous layer - Adenomyosis
30% in ovary and pelvic peritoneum
Aetiology
Delay in child bearing
Less use of OCs
Exposure to environmental toxins such as dioxins
Familial tendency
Vaginal or cervical atresia which encourage retrograde spill
Sites of Endometriosis
Pelvic
Umbilicus
Scars (Lap)
Lungs and pleura
Risk Factors
First degree relative of affected person
Short menstrual cycles
Log duration of mentrual flow
Low parity
Infertility
Fair complexion
Pathophysiology
1. Implantation Theory
Retrograde menstruation - reflux of the menstrual flow through the fallopian tubes into the peritoneal cavity - proof: scar endometriosis following classical caesarian section, hysterectomy, myomectomy and episiotomy
2. There is a combination of failure of immune mechanisms associated with stromal cell defect with its increased oestrogen, prostaglandin and progesterone resistance
3. Coelomic metaplasia theory
Endometriotic lesions develop when coelomic mesothelial cells of the peritoneum undergo metaplasia
4. Metastatic theory
the circulation and implantation of ectopic mestrual tissue via the venous or the lymphatic system or both, to sites like the umbilicus, pelvic lymph nodes, ureter, rectovaginal septum, bowel wall, and remote sites like the lung, pleura, endocardium and the extremities.
Hormonal influence
the activity of endometriosis is influenced by hormones ; estrogen aggravates and progesterone mitigates it.
Pregnancy atrophies the endometriosis - effect of progesterone
Oophorectomy irradiation menopause and hormones with antiestrogenic activity cause regression
Immunological Factor
Peritoneal fluid in endometriosis shows the presence of macrophages and natural killer ( NK ) cells
Impaired T cell and and NK cell activity and altered immunology may cause endometriosis
Pathology
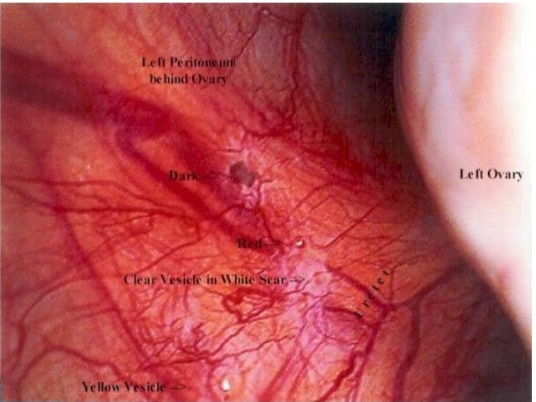
1. Superficial peritoneal lesions : on the pelvic organs or pelvic peritoneum
Bluish or blue-black "powder-burn" lesions; may be associated with hemosiderin deposits.
Papular and red vesicles filled with haemorrhagic fluid
Yellowish-whte thick plaques - healed lesions
Clear and red "flame-like" lesions or white lesions -
Scarring - puckering
Chocolate cysts
Vascular red adhesions on the under surface of the ovary
2. Endometrioma
Clinical Features
Chronic pelvic pain
Worsening dysmenorrhea
Acquired dyspareunia
Infertility
Prementrual spotting
Dyschezia
Bimanual pelvic exam : fixed retroverted uterus, bilateral pelvic tenderness, fixed or enlarged ovaries and painful uterosacral nodularity
Deeply infiltrating nodules felt by PV during menstruation
Adenomyotic enlarged uterus, soft smooth and tender
Investigations
Lap
USGM
MRI
Ca 125
Histological cofirmation especially if in ovary to R/O malignancy
Classification/Staging
Stage I : minimal score 1-5
Treatment Recommended for
Stage II : 6-15
Stage III : 16 - 40
Stage IV : > 40
Treatment Considerations
Age
Symptoms
Stage
Infertility
Goals
Pain Management
Preservation / Restoration of Fertility
Discuss with patient : disease may be chronic and not curable
Optimal treatment unproven or nonexistent
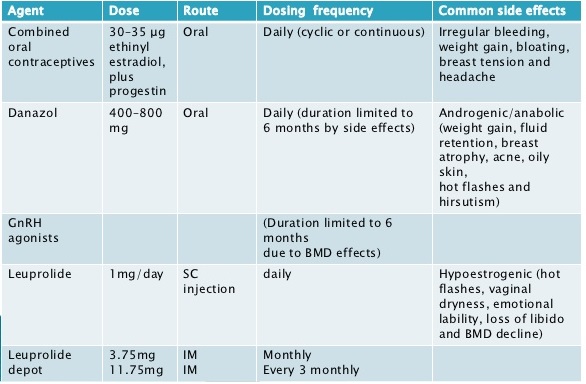
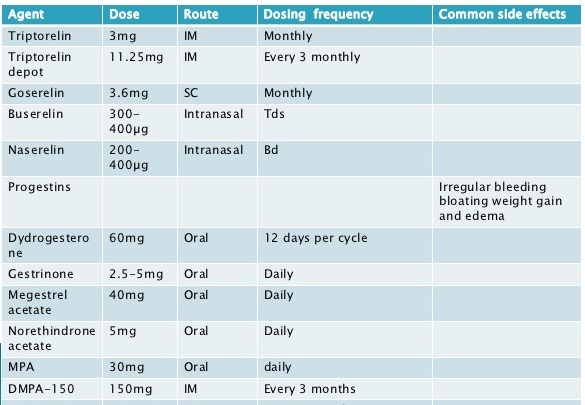
Medical Management
Empirical treatment of pain symptoms without definitive diagnosis
Therapeutic trial of hormonal drugs
Can be combined with surgery- preoperatively or post-operatively - sandwitch therapy
NSAIDs
GnRH analogues - pseudo menopausal state
Danazol - 400 mg/day
Progesterone - Pseudo pregnancy state (Kristner's Regime)
DMPA
LNG-IUS (Mirena)
Gestrinone : androgenic, progestogenic and antiestrogenic
C;ombined OC pills
RU 486
Aromatase inhibitor
Interferons
SERMs
Surgical Management
Indications
Mild endometriosis associated with infertility
Endometrioma > 4 cm dia
Endometriosis of rectovaginal septum or rectal wall
failed medical therapy - or if intolerable side effects
Endometriosis with other surgically correctible infertility factors
Preoperative Assessment
MRI
USGM
IVP
Ba enema
Sigmoidoscopy
Preoperative ad postoperative medical management
GnRh - goserili for 3 months preoperatively
Primary operation is the best opportunity
Excision of the lesion
Adhesion release
Carbon-di-oxide or Nd YAG laser use
Harmonic scalpel
Argon beam for widespread lesion
Helica thermal coagulator
Surgery when infertility is the priority
Early stage : Lap excision or ablation with adhesiolysis
Moderate to severe stage : role of surgery is uncertain; endometrioma - laparoscopic cystectomy, tubal flushing
Assisted Reproduction in Endometriosis
IUI
IVF
GnRH agonists
IVF
Laparoscopic ovarian c;ystectomy
* * * * * * * * * * * * * * *
ANNABELLE D MARIE & https://www.slideshare.net/elnashar/endometriosis-37404999
Revised American Fertility Society Classification of endometriosis 1985 Patients name Age Date Stage I (Minimal) Score 1-5 Laparoscopy/Laparotomy/Photography Stage II (Mild) Score 6-15 Recommended treatment Stage III (Moderate) Score 16-40 Stage IV (Severe) Score > 40 Total PrognosisPeritoneal endometriosis <1 cm 1-3 cm >3 cm Superficial 1 2 4 Deep 2 4 6Ovarian endometriosis <1 cm 1-3 cm >3 cm Right/Left side separate points Superficial 1 2 4 Deep 4 16 20cul-de-sac obliteration Partial Complete 4 40Ovarian adhesions <1/3 Enclosure 1/3 to 2/3 Enclosure >2/3 Enclosure Right/Left sideseparate points Flimsy 1 2 4 Dense 4 8 16 Tubal adhesions <1/3 Enclosure 1/3 to 2/3 Enclosure >2/3 Enclosure Right/Left sideseparate points Flimsy 1 2 4 Dense 4 8 16
21. ? Age.? Symptoms.? Stage.? Infertility
22. ? Recognize Goals: – Pain Management – Preservation / Restoration of Fertility? Discuss with Patient: – Disease may be Chronic and Not Curable – Optimal Treatment Unproven or Nonexistent
23. ? Management of Endometriosis must be ‘tailor made’ taking into account, patients profile, presenting symptoms, impact of the disease and effects of treatment on day to day life.