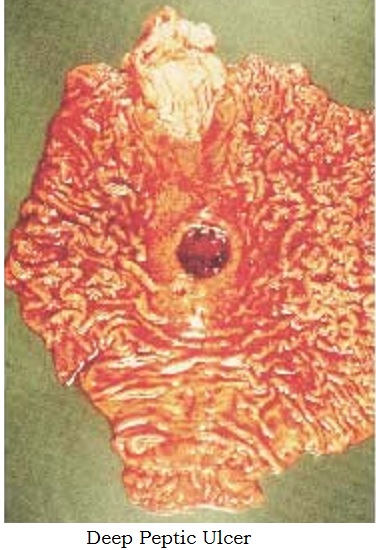
Peptic Ulcer
Definition
Break in the epithelium & Excavation formed in the mucosal wall of the oesophagus, stomach, pylorus or duodenum.
Aetiology
H.pylori infection (70% 95%) (gram negative bacteria)
Excessive acidity (Zollinger-Ellison Syndrome)
Stress
Caffeinated beverages
Smoking
Alcohol
Familial tendency
Blood type 'O'
NSAID
Gastrin
Gasro-oesophageal reflux
Pathophysiology
Ingestion of food - acetylcholine, gastrin and histamine bind to specific receptors of the parietal cells in the fundus of the stomach & secrete hydrochloric acid.
The parietal cells with the the assistance of the hydrogen - potassuum adenosine triphosphatase (H+, K+ - ATPase) pump (Proton Pump) transport the hydrochloric acid to the stomach lumen
Chief cells in the stomach secrete pepsinogen, which converts to pepsin in the presence of hydrochloric acid.
Pepsin breakdowns the food
Mucous barrier from duodenal cells in the gastric epithelium protects the lining of the gastroduodenal area.
Increased action of acid-pepsin or decreased resistance of the mucosa.
Damaged mucosa cannot produce enough mucus barrier against acid
NSAID inhibits secrerion of this mucus
ZES gastrinomas (islet cell tumours ) in the pancreas - gastrin - increased secretion of acid - multiple ulcers or ulcer intractable.
Stress ulcers are different from Cushing's ulcers and Curling's ulcers
Cushing's ulcers - trauma to the brain
Curling' ulcers - extensive burns
Stressful conditions like burns, shock, severe sepsis, multiple organ trauma - post surgical conditions ' multiple erosions. Shock - decreased blood flow to stomach mucosa., reflux of duodenal contents into the stomach. Large quantities of pepsin released. Combination of ischaemia, acid and pepsin - ulceration
Clinical Manifestations
Dull gnawing pain or a burning sensation in the midepigastrium or in the back.
Pain relieved by eating
Night pain morning relief
periodicity
Sharply localized tenderness in the epigastrium slightly to the right of the midline
Heartburn (pyrosis)
Vomiting
Constipation
Diarroea
Bleeding
Melena (altered blood in the stool) black tarry stools
Haematemesis (ground coffee coloured vomitus)
Vomiting of food which was consumed two to three days earlier in pyloric stenosis. (gastric outflow obstruction)
Asymptomatic ulcers
Asymptomatic ulcers which perforate
Differential Diagnosis
Amoebiasis
Gall stones
Cholecystitis
Pancreatitis
Investigations
Hb , TC, DC, ESR
Upper GI endoscopy (Choice)
Gastroscopic biopsy in appropriate cases and histopathological examination and tests to detect H.pylori infection : culture,
Barium meal
Stool for occult blood
Breath test that detects H.pylori
Serological tests to detect antibodies against H.pylori
Medical Management
Inform that remissions and recurrences are common
Eradication of H.pylori - an antibiotic, a proton pump inhibitor and metronidazole (Ulcikit, Zovanta Kit, H.pylori kit)
Histamine receptor antagonists (H2 receptor antagonists), cimatidine - ranitidine - famotidine
Proton pump inhibitors which also decrease acid secetion from acid or NSAIDs - omeprazole, pantoprazole, rameprazole, rabeprazol
Antacids - gelusil, ulgel, mucaine gel, etc containing aluminium hydroxide
Cytoprotective Medicationss - misoprostol, sucralfate
Rest, sedatives, and tranquilizers
Maintenance dosages of H2 receptors antagonists ae usually recommended for one year
ZES - H2 receptor antagonists. Twice the normal dose. Octreotide (sandostatin, a medication that suppresses gastrin levels )
Stress - IV H2 receptor antagonists and cytoprotective agents
Change of life style
Stop smoking
Dietary modification bland diet and avoidance of offending food.
Surgical Management
Has become rare with the arrival of newer drugs
Procedures which were use in the past are
1. Gastrojejunostomy
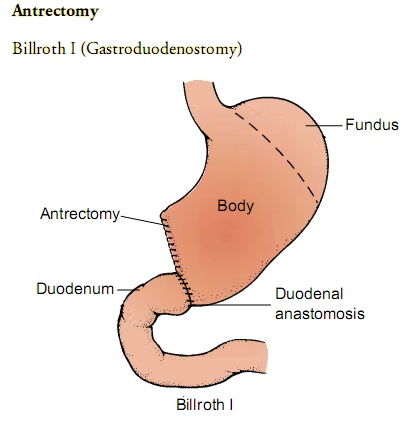
antrectomy with gastroduodenostomy - Billroth I
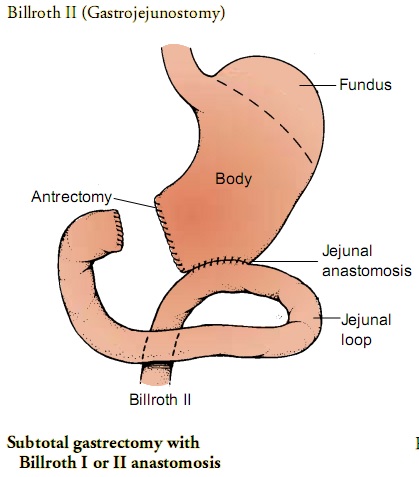
o Antrectomy with gastrojejunostomy - Billroth II
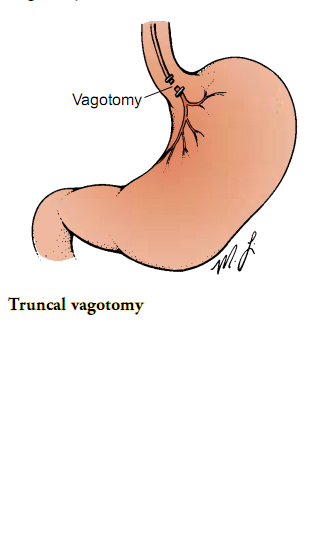
o GJ Vagotomy - truncal, selective, highly selective
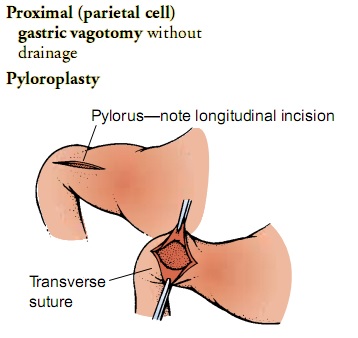
o GJ Vagotomy with pyloroplasty
Complications of Peptic Ulcer
Haemorrhage
Perforation
Penetration
Pyloric obstruction (gastric outlet obstruction)
Perforated peptic ulcer - gas under diaphragm
University Questions
Thiru.Somanath aged 35 years is a business executive. He is admitted with acute abdominal pain. Hi is diagnoses as peptic ulcer with perforation.
o How do you prepare the patient for emergency surgery?
o Describe the post-operative nursing management of the patient for the 1st 24 hours.
Preparation for Emergency Surgery
Patient need not be rushed to the O.T. though it is an emergency surgery - upto 6 hours can be spent on improving the general condition
Make the patient comfortable in bed
Start IV fluids to correct fluid and electrolyte imbalance
Do investigations : CBC, ESR, Blood urea, serum creatinine, BT, CT, Serum electrolyte estimation, Plain X-ray Chest to look for air under diaphragm, plain X-ray abdomen
Monitor vital signs : TPR frequently
Monitor Abdominal girth 4 hourly
Monitor SpO2 by pulse oxymetry
Start Pain relieving drugs - if needed narcotics
Start antibiotics and imidazole derivatives (Ciprofloxacin/Ofloxacin + Metronidazole/ornidazole Or Cefaperazone + Sulbactum (inj.Magnex) +Metronidazole)
Insert Ryle's tube and start continuous or freuent nasogastric suction
Administer Inj.TT and Lidocaine sensitivity test
Clean and prepare the abdomen for surgery Laparoscopic / open
Post operative management for the first 24 hours
Semi-Fowler's position to relax incision
Pain relief with Narcotics or Tramadol
Maintain fluid and electrolyte balance
Continous Nasogastric suction
Monitor abdominal girth
Cough : support the incision with hands
Antibiotics and other medications, Proton pump inhibitors
Watch for bleeding from the site of surgery
4th hourly TPR
Monitor SpO2 by pulse oxymetry
ECG monitoring
I/O chart
Monitor urinary output
Deep breathing encouraged
Early ambulation when possible