Induction of Labor
List the indications for innduction of labor
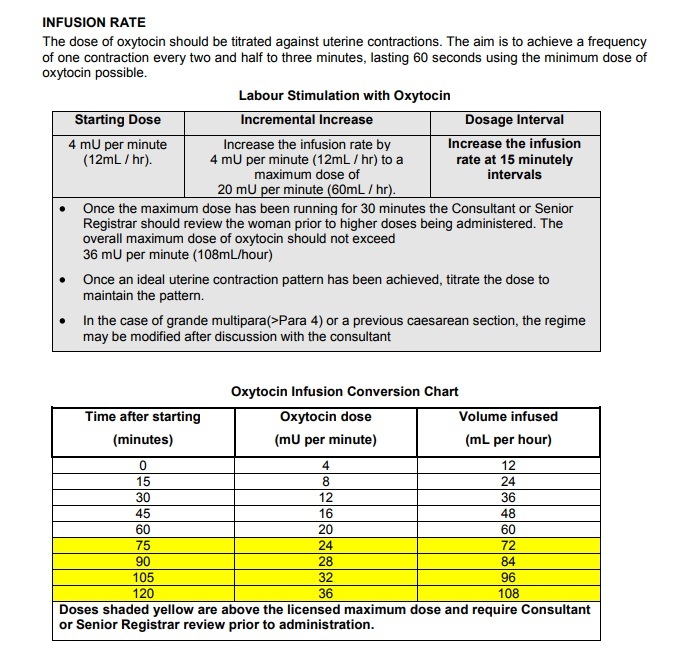
Explain the management and care of a woman on oxytocin infusion for induction.
Definition
Artificial initiation of labor mechanism prior to its spontaneous onset
Indications
Premature rupture of membrane - prolonged
Prolonged pregnancy (Post-term) - Main indication
Preterm premature rupture of membrane
Pre eclampsia (PIH), Eclampsia
Maternal medical illnesses like diabetes with placental insufficiency, uncontrolled DM
Chronic renal disease
Rh-isoimmunisation
Abruptio placentae
Fetus with congenital anomaly
Intra uterine death
Contraindications
Contracted pelvis and CPD
Malpresentations
Previous classical caesarean section & hysterotomy
Uteroplacental factors : unexplained vaginal bleeding, vasa previa, placenta previa
Cord presentation, cord prolapse
Active genital herpes infection, HIv
Pelvic tumor
Preparation
Time of induction : preferably early morning
Place of induction : Where facilities for intervention and fetal monitoring is available
Preparation of patient : enema may be given
Factors to assess prior to induction
Maternal Assessment :
Confirm the indication
Exclude the contraindications
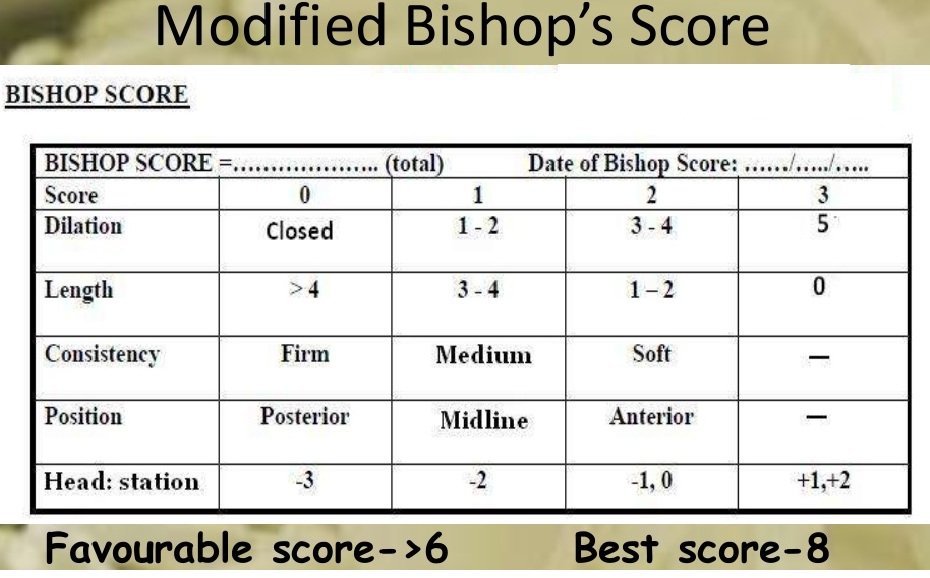
Assess Bishop score
Assess pelvic adequacy
Fetal Assessment
Fetal gestational age
Fetal presentation
Fetal well being
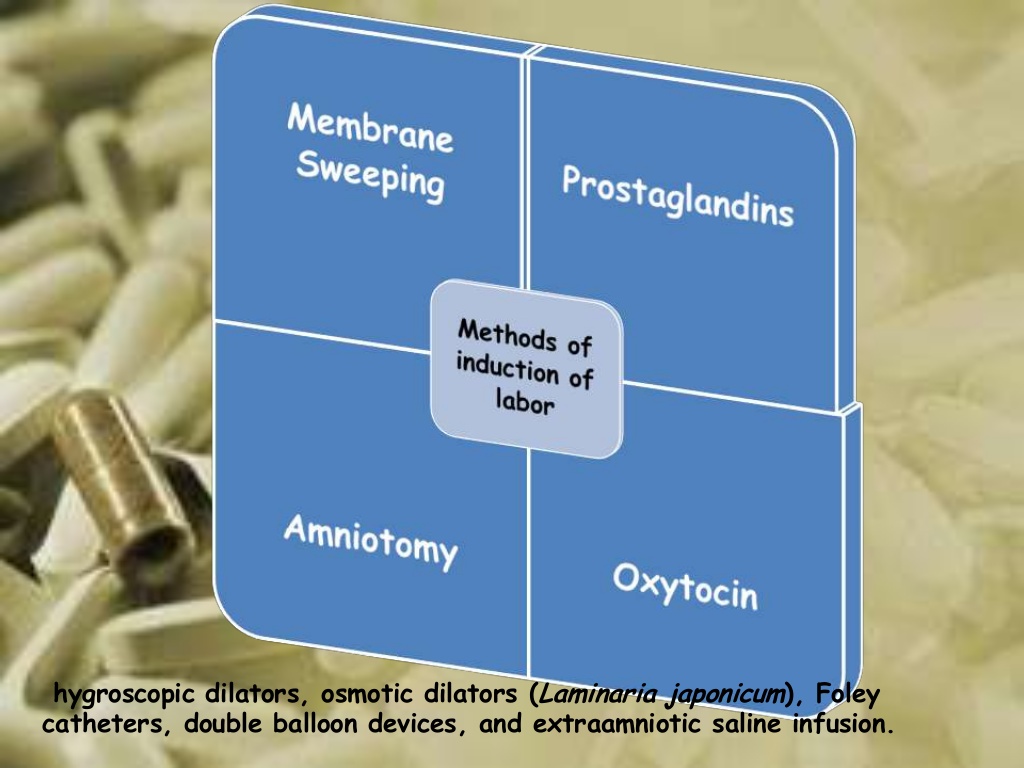
Methods of Induction of Labor
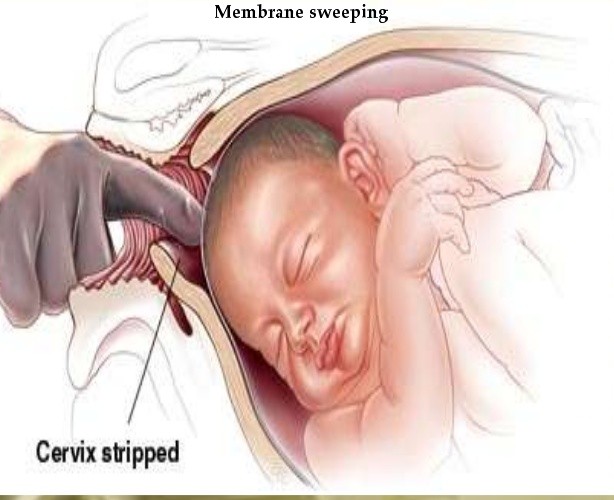
Membrane sweeping - if the cervix has ripened enough to allow the passage of a finger - finger is inserted and the membranes separated from the uterine wall the pressure always being on the uterine wall. It strips the chorioninc membrane from the underlying decidua leading to release prostaglandins. Ensure there is no placenta previa.
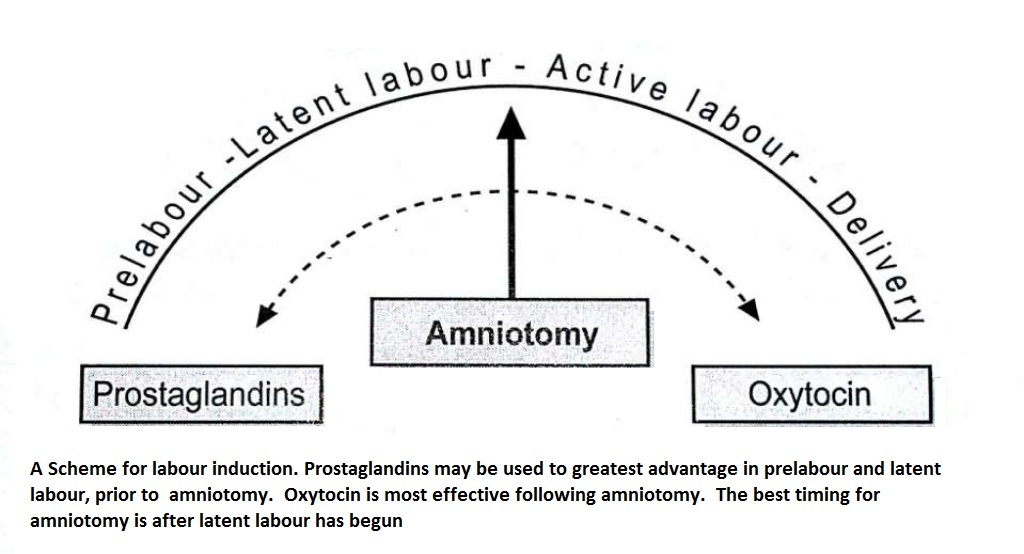
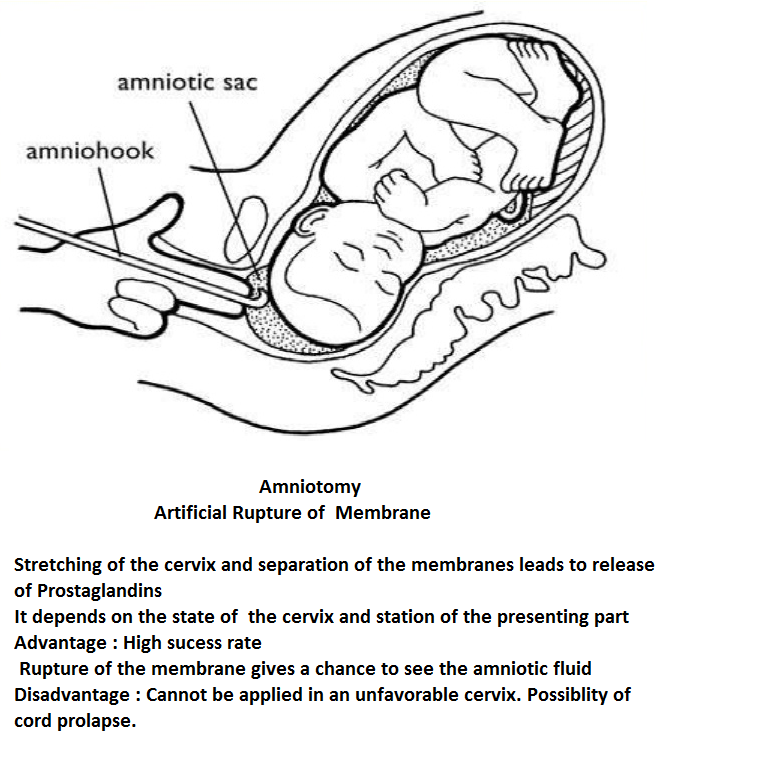
Amniotomy - this is artificial rupture of the membranes. - it may be preceded by prostaglandins in prelabor and latent labor - cannot be applied in an unfavourable cervix - it is contraindicated in IUD, HIV - complications : cord prolapse, amnionitis, amniotic fluid embolism, abruptio placentae
Prostaglandins : Administration of prostaglandins sensitises the myometrium to the oxytocin and ripens the cervix. thpes of prostaglandins :
PGE1 from amnion PGE2 from amnion PGF2 from dicidua and myometrium PGI2 from myometrium.
Prostaglandin used : PGE1 (Misoprostol) and PGE2 (Cerviprime) - Contraindications bronchial asthma, pulmonary disease, previous uterine scar.
Misoprostol : Dose of 25 microgram every 4 hours to a maximum of 6 doses intravaginally/Dose of 50 micrograms every 3 hours to a maximum of 6 doses orally/Dose of 25 micrograms every 2 hours orally to a maximum of 6 doses
The chances of fetal distress is less with oral administration than with the vaginal but oral administration is less effective than the vaginal
Dinoprostone : Vaginal gel of 0.5 mg intracervically, may be repeated after 6 hours x 3-4 doses
Vaginal tabs of 3 mg in the posterior fornix; one more dose after 6-8 hours; max- 6 mg
Vaginal pessary 10 mg for 24 hours. To be removed when cervix is adequately ripened
Oxytocin: (Syntocinon) Commonly used- produces uterine contractions and effective in producing changes in cervix and in the descent of the presenting part; commonly IV route is preferred. maximum doseof oxytocin : 5IU in 500 ml of fluid at the rate of 40 drops/min. Started with 10 drops and increased to 20, 30 and 40 gradually.
* * * * * * * * *
PRIOR TO COMMENCING OXYTOCIN
Oxytocin should not be started for six hours following administration of vaginal prostoglandins.
For women with intact membranes an ARM should be performed prior to commencing induction.
Establish fetal well-being immediately prior to commencement of oxytocin.
Perform a 20-30 minute cardiotocograph (CTG) prior to commencing the induction.
Women with a previous caesarean section scar should have discussion and consent to the use of oxytocin. The rupture risk (approximately 1:100) should be explained and this discussion documented in the medical notes.
Standard Dilution of Oxytocin
10 I.U. of oxytocin in 500mL of Hartmannís solution.
At this dilution, a 3mL/hr infusion rate equates to 1milli-unit (mU) of oxytocin per minute.