Osteoarthritis
Definition
A type of degenerative joint disease
Result of breakdown of joint cartilage and the underlying bone.
Incidence
Osteoarthritis is the most common form of arthritis.
Over 60 years of age; by the age of seventy five percent of the population affected. But only 15 % to 25% experience have significant symptoms.
10% of males and 18% of females affected.
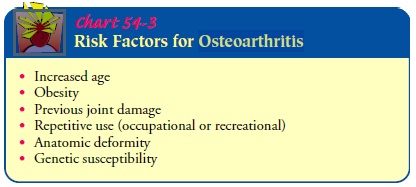
Aetiology
Primary or Secondary
Previous joint injury
Abnormal joint or limb development
Inherited factors
High levels of joint stress
Overweight
Congenital defects in the joints
Clinical Features
Pain in the joint
Swelling
Joint stiffness
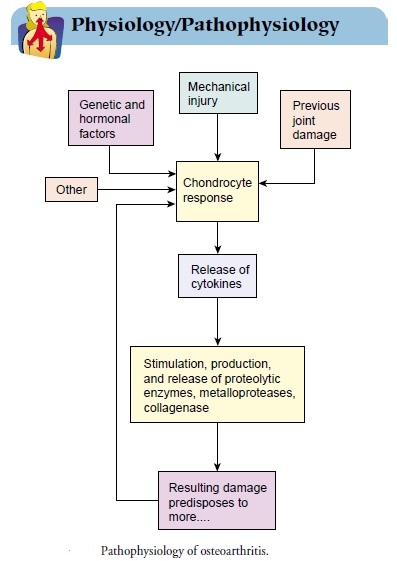
Pathophysiology
There is a generalized predisposition to the disease
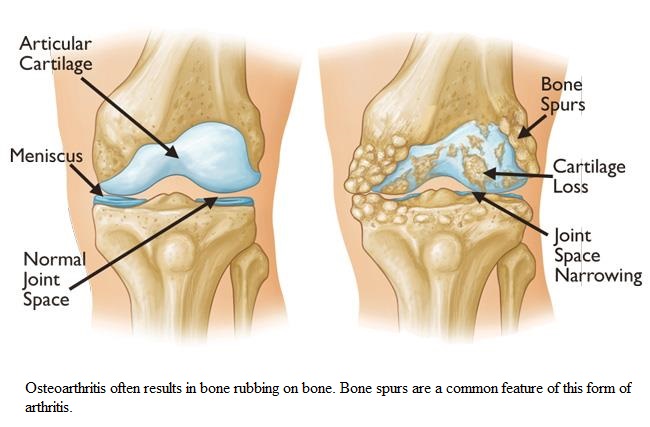
Joint cartilage degrades
Subchondral bone stiffens
There are microfractures in the cartilage and the subchondral bone
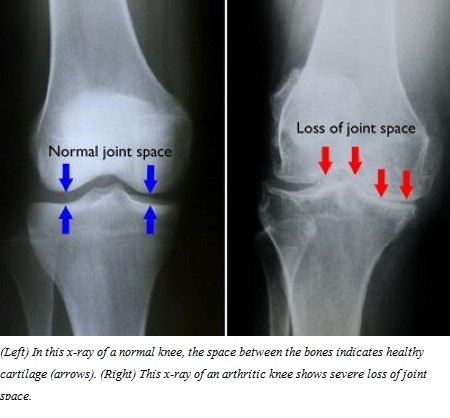
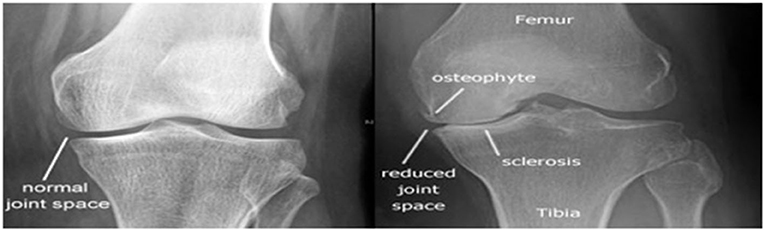
Progressive loss of cartilage is seen as reduction of joint space in the X-Ray
Reactive changes occur at the joint margins as the cartilage attempts to regenerate, seen as osteophytes or spurs
Reactive inflammation occurs in the synovium of the joint
Pain due to inflammation of the synovium, stretching of the joint capsule or ligaments, irritation of nerve endings in the periosteum over osteophytes
Inflammation of the bursa, tendons and muscular spasm add to the pain
Clinical Manifestations
Joint pain
Stiffness - mostly experienced in the morning or after awakening; usually lasts less than 30 minutes and decreases with movement.
Functional impairment
OA occurs most often in weight bearing joints
in hips, knees, cervical and lumbar spines
the proximal and distal finger joints are also often involved
The joints are enlarged
Bony nodes may be present on inspectiona and palpation; these are usually painless, unless inflammation is present.
Though changes are present in the X-Ray are present only 30% to 50% report symptoms
Diagnosis
History, physical examinations, X-ray of the knee (the involved joint) to find out any joint space reduction, cysts and thickenings of the bones (osteophytes)
Other investigations
CT scans, MRI scans, blood investigations to R/O systemic diseases like rheumatoid arthritis, gout, or any infection. Arthrocentesis : synovial fluid subjected to lab tests.
Medical Management
No treatment halts the degenerative process
Certain preventive measures can slow the progress :-
Use of heat, weight reduction, joint rest avoidance of joint overuse, orthotic devices to support inflamed joints (splints, braces), isometric and postural excercises and aerobic eexcercises
Occupational and physiotherapy for self management strategies
Pharmacologic Therapy
Acetaminophen
NSAIDs
COX-2 inhibitors
Opioids
Intra-articular corticosteroids
Topical analgesics such as capsaicin and methylsalicylate
Glucosamine and Chondroitin
Viscosupplementation, the intra-articular injection of hyaluronic acid
Surgical Management
Osteotomy and arthroplasty (joint components are replaced with artificial products)
Viscosupplementation (reconstitution of synovial fluid viscosity).
Tidal irrigation
Nursing Management
Pain relief first by non pharmocological and then pharmacological means are added
Optimize functional ability
Educate the patient about the disease process and symptom pattern
Encourage aerobic activities such as walding
Quadriceps strengthening exercises
Physiotherapy when needed
Assistive devices like walking sticks or similar devices
Exercises at a time when the pain is least
If needed an analgesic before exercising
* * * * * * * *
Viscosupplementation (the reconstitution of synovial fluid viscosity). Hyaluronic acid (Hyalgan, Synvisc), a glycosaminoglycan that acts as a lubricant and shockabsorbing fluid in the joint, may be used in this procedure. Hyaluronic acid stimulates the production of synoviocytes, possibly providing better and more prolonged pain control. A series of three to five weekly intra-articular injections are given. Pain relief may last for 6 months.
Tidal irrigation (lavage) of the knee involves the introduction and then removal of a large volume of saline into the joint through cannulas. In some cases it provides pain relief for up to 6 months
The diagnosis of osteoarthritis is made based on history, physical examination, and radiological evidence. A detailed history regarding the onset of symptoms and associations is taken, which is followed by a physical examination of the involved joints. Blood investigations may be done to rule out systemic diseases such as rheumatoid arthritis, gout, or any infection.
Plain radiographs are usually the first radiological test done to look for joint space reduction, cysts, and thickening bones. In some cases, for a detailed evaluation, a CT scan or an MRI may be ordered. An MRI gives the details of all the soft tissue structures inside the joint, which are not visible on an X-ray.
In some cases, joint aspiration or arthrocentesis may be done, which involves taking a tiny amount of synovial fluid from the joint using a syringe. The contents of synovial fluid are then subjected to lab tests.
The management of osteoarthritis depends on the severity of the disease and the lifestyle limitation as a result of the disease. Non-surgical treatment forms the first line of management that involves weight loss, physical therapy, cold and heat therapy, and nonsteroidal anti-inflammatory medications.
Intra-articular steroid injections may be administered in the joint by the surgeon. Intra Articular steroid injections decrease the inflammation associated with osteoarthritis. Significant pain relief is obtained, but the effects wear off after a few months.
Repeat injections may be needed. Certain medications such as glucosamine, chondroitin sulfate, diacerein, and hyaluronic acid have been used, but controversies surround their actual benefit.
The surgical management may involve procedures such as arthroscopic debridement of the joint in the early stages of osteoarthritis. Arthroscopic debridement involves the use of a keyhole incision through which a tiny camera is inserted along with instruments. All the dead tissues and loose bodies are removed.
In large joints such as the knee joint, bone-cutting surgery known as osteotomy may be done to change the alignment of the forces acting on the joint. It decreases the pressure on the area of the cartilage involved in osteoarthritis, but it is only helpful in the early stages of the disease.
Osteoarthritis is a progressive disease that continues to progress despite interventions, and ultimately most patients may require joint replacement surgery. Joint replacement surgery has revolutionized the management of osteoarthritis. The joint ends are replaced or resurfaced with metal and plastic parts.
The prosthetic parts recreate the joint movements. The alignment of the joint line is created as it was before the disease process. Joint replacement provides a pain-free joint with a near-normal range of motion. Recent advances have ensured that most artificial joints last 15-20 years or more.